State of Veteran Mental Health and Substance Abuse in America
Across America, perhaps no one single group of people sacrifice more for their country than our military—both active duty and retired Veterans who at some point in their lives were willing to give up everything to protect and defend their nation.
At the same time, the suicide rate among American Veterans has increased by 25 percent in the last decade, making them more in danger of mental health disorders than the population at large. With over 23 million Veterans across the country, studies suggest that only half of returning service members who need treatment for their mental health actually seek care, and substance abuse continues to mark a growing concern among both enlisted and retired members of the armed forces.
To learn more about the immediate nature of this growing tragedy, we’re analyzing 2017 Behavioral Risk Factor Surveillance System (BRFSS) data from the Centers for Disease Control and Prevention (CDC). Our study takes a close look at the dangers of binge drinking among Veterans, drunk driving incidents, and the emotional and physical trauma that could be leading to this substance misuse among some of America’s most dedicated heroes. Read on to learn more.
Overconsumption of Alcohol
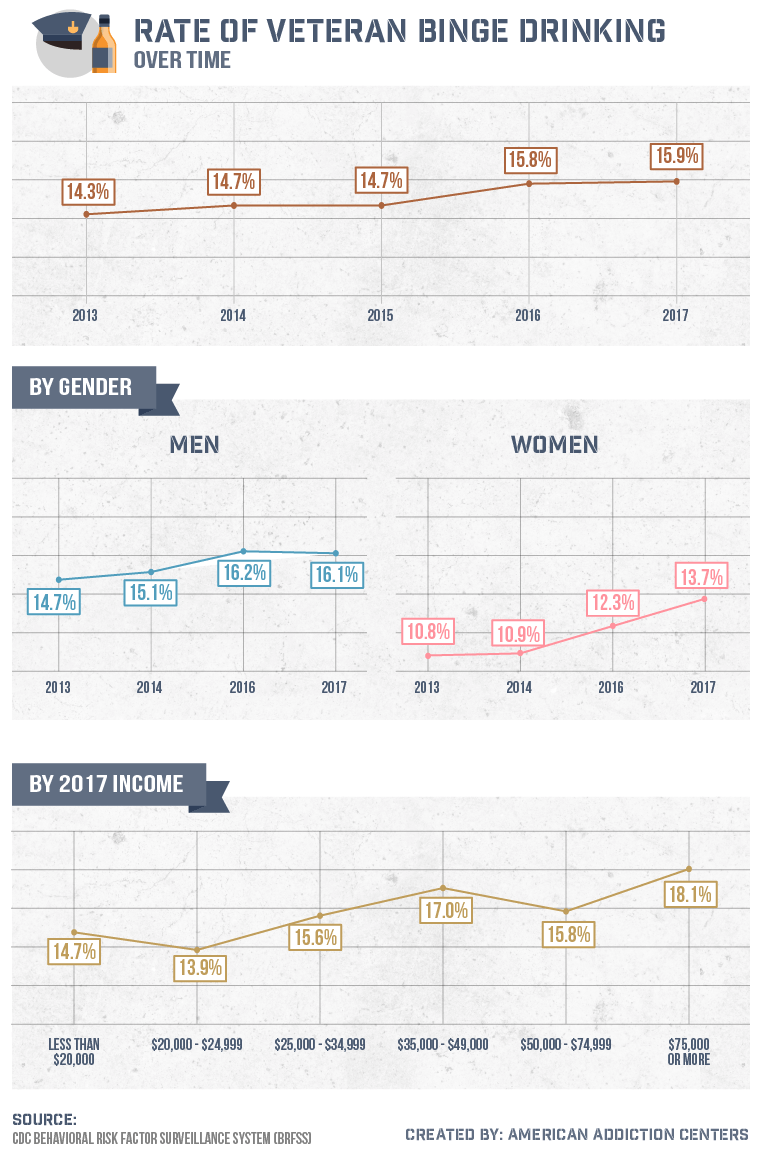
Since 2013, the number of Veterans who’ve been diagnosed with episodes of binge drinking has increased from roughly 14 percent to nearly 16 percent. But as our analysis shows, binge drinking among veterans may affect certain subsets of service members far more than others.
Typically defined as consuming more than four drinks within a two-hour period for women and five drinks for men, binge drinking can lead to severe mental and physical health concerns. Roughly half of all alcohol-related deaths in America are related to extreme consumption, and in addition to alcohol poisoning and rapid cognitive decline, even just a single night of heavy drinking may cause lasting damaging effects on parts of the body, including the heart, liver, lungs, and brain.
While binge drinking among Veterans was more common with servicemen than women, we found the rate of increase was higher among female Veterans overall. Compared to a less than 2 percentage point increase between 2013 and 2017, the rate of binge drinking among women rose from less than 11 percent to nearly 14 percent over the same five years. In 2017, binge drinking among America’s Veterans was highest among those earning the most annually, including more than 18 percent of men and women making $75,000 or more every year.
Regional Assessment of Alcohol Consumption
Overwhelmingly, research suggests the biggest factor leading to substance abuse and dangerous drinking habits among Veterans is post-traumatic stress disorder. Service members who exhibit PTSD symptoms are more likely to be linked with drinking problems overall. For example, evidence suggests as many as 60%–80% of Vietnam War Veterans may have alcohol use disorders and a higher occurrence of binge drinking. Sadly, the same studies suggest alcohol consumption is more likely to exacerbate the conditions of PTSD rather than help abate them.
Across the country, binge drinking among American Veterans was highest in Hawaii (21.5 percent), Nevada (20.5 percent), and Wisconsin (20.1 percent). In 2017, Hawaii received a $3 million federal grant to help combat substance abuse and mental health disorders across the various islands that make up the state with a combination of both Western treatment plans and their own cultural influence to help humanize the recovery process.
In contrast, it was states like Utah (9.1 percent), West Virginia (9.6 percent), and Mississippi (10.2 percent) that had the lowest reported occurrences of binge drinking among veterans. While Veterans may be at lower risk in Utah, the statewide approach to drinking and addiction still has work to do. At least one study predicts Utah will experience a sharp rise in deaths related to alcohol, drug use, and suicide in the coming decades.
Buzzed Behind the Wheel
In 2016, more than 10,400 people died across the country as a result of alcohol-related crashes, and roughly 1 million drove under the influence. When combined, these findings suggest 29 people die every day in car accidents that involve a driver under the influence of alcohol—or one person every 50 minutes.
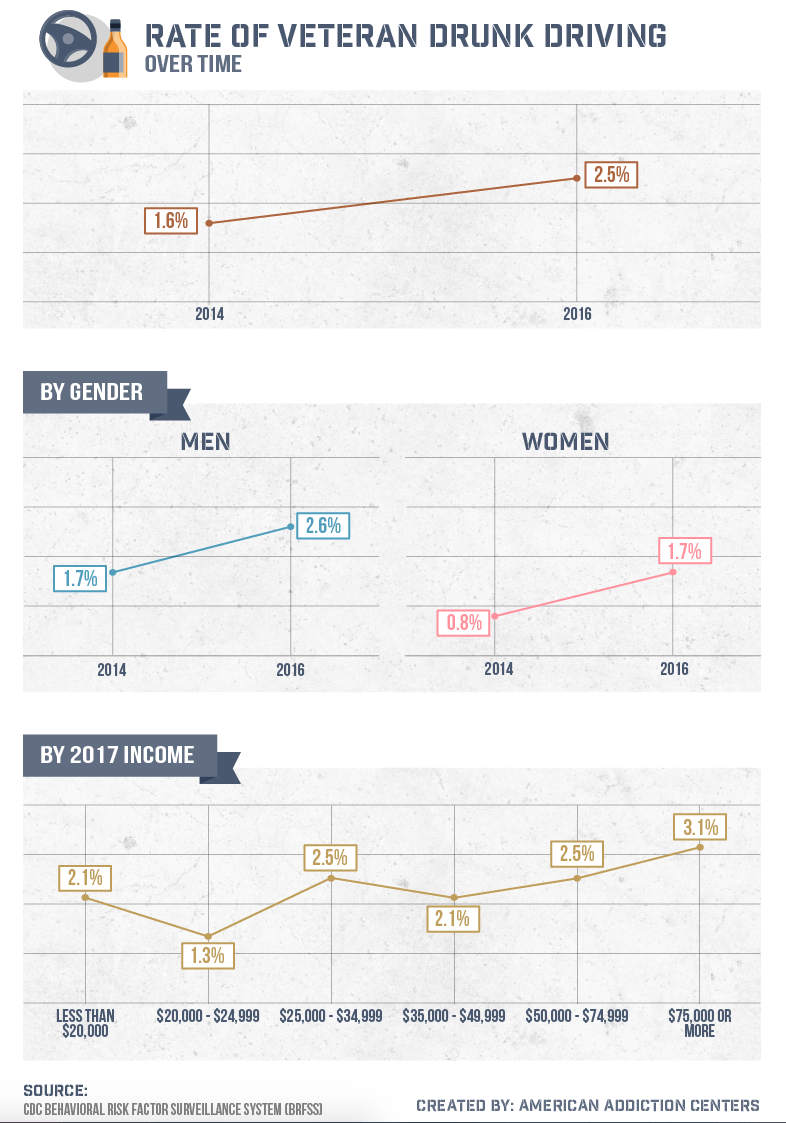
And even though some officials are trying to pass legislation that would allow Veterans to avoid conviction in charges associated with driving under the influence, there’s no denying that American Veterans contribute to the nationwide epidemic of drunk driving. Since 2014, the percentage of U.S. Vets identified as driving while drunk increased from 1.6 percent to 2.5 percent. Those rates were concurrently higher among men than women but were highest among Veterans of both genders earning $75,000 or more in 2017 (3.1%).
Regional Analysis of Dangerous Driving
The consequences of driving under the influence can be deadly (and not always solely for the offending party), but not all states approach DUI convictions the same way. In some regions, the driver might only be required to pay a fine for drinking and driving, while others mandate minimum jail sentences instead.
States like Georgia, Texas, and California typically have the strictest DUI laws, but that doesn’t necessarily mean they have the lowest rate of alcohol-related crashes or fatalities. Specifically among Veterans, California (9.1 percent) had the highest percentage of drunk driving occurrences in 2016. While California represented the highest rate by far, Kentucky, Washington, D.C., Illinois, and Connecticut also ranked among the most common states for drunk driving involving Veteran service members.
Emotional Impact on Alcohol Abuse
Substance use, depression, and other co-occurring mental health disorders are common among armed service members. Particularly among those who serve abroad, the likelihood of PTSD or related mental health conditions is significantly higher than the standard population. Studies suggest that 30 percent of Veterans who served in Iraq and Afghanistan may have returned home with mental health issues that put them at a much higher risk for suicide and depression. Unfortunately, those same service members may not have consistent quality access to care that could successfully address all of their needs.
Instead, alcohol abuse and binge drinking are higher among Vets who identify as depressed compared to those who don’t. In many cases, addiction can become a coping mechanism for trauma or depression. Moreover, the percentage of depressed Veterans who at some point have been involved in an episode of binge drinking increased substantially between 2014 and 2016. Compared to the roughly 15 percent not linked to depression who were identified as binge drinkers, more than 1 in 4 American Veterans who self-identified as depressed were linked to binge drinking. Perhaps even more dangerous, Veterans with depression are more than twice as likely to be linked with drunk driving compared to those without similar mental health concerns.
Mental Health Concerns
For people of all walks of life, depression often occurs after a trauma. That may not always be the case (mental health concerns like depression have also been identified as a hereditary condition for some), but particularly among service members, those suffering from PTSD are typically three to five times more likely to experience depression. In most cases, depression and PTSD also happen to exhibit many of the same symptoms.
Between 2014 and 2016, the depression rate among female Veterans in America fell sharply from 47 percent to 37 percent, causing the total percentage to decrease slightly from 28.2 percent to 27.7 percent of Vets who’ve been linked with depression. Over that same period of time, instead of declining, the depression rate among men increased from 26.2 percent to 27 percent in 2016. And while major mental health concerns varied among service members with different annual salaries, it was the unemployed (40 percent) and those disabled and unable to work (68 percent) who were most commonly linked with depression. In 2016, more than 450,000 of the nearly 21 million U.S. Vets were unemployed and looking for work.
Long-Term Effects of Service
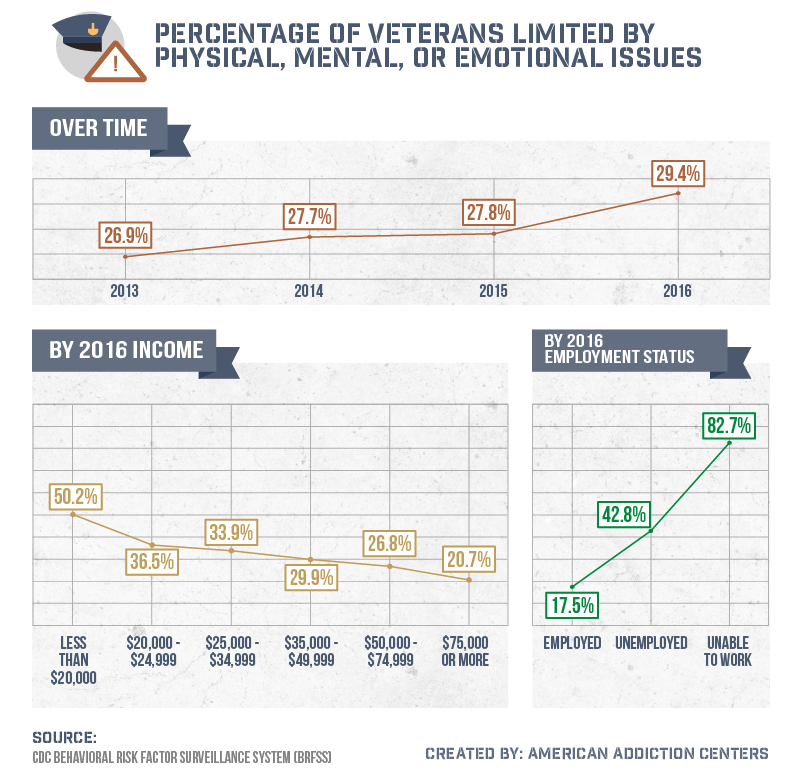
In 2016, roughly 621,000 Vets qualified for some level of disability as a result of their service and the physical and emotional trauma they may have suffered. Since 2013, the percentage of Veterans who are limited by this health concern had risen from less than 27 percent to over 29 percent.
And while that increase may seem small at first, it’s important to recognize that Veterans who are limited by consequences of their service typically fall within the lowest income percentiles (more than half of those earning less than $20,000 experience disability) and are simply unable to work. In 2016, more than 4 in 5 Vets citing an inability to work were limited either physically or mentally following their service in the armed forces.
Getting Vets the Help They Need
The men and women in America who volunteer to be a part of the armed forces recognize the level of sacrifice associated with their service. From the amount of time they dedicate to their respective branch of the military to stresses on their body and mind, there’s nothing easy about the work they do. Still, many leave their service with either physical or emotional trauma (or both) that may cause depression or even thoughts of suicide. As our analysis revealed, that depression may have a very strong correlation to the rising number of Vets linked to binge drinking and drunk driving.
If you or someone you know needs help dealing with suicidal thoughts, help is available 24/7.
Call the National Suicide Prevention Hotline at 1-800-273-8255.
Veterans can also utilize the Veteran Crisis Line via text 838255 or via online chat with a crisis counselor.
No matter who you are or what walk of life you come from, help is always here for you. At Desert Hope Treatment Center, our mission is to help men and women across the country learn more about the disease that is addiction and find the support and treatment they need to live their best lives again. If you or someone you love is battling drug or alcohol alcohol, let us help you find the care you need.
Call us at today to learn more about substance abuse treatment in Las Vegas, Nevada.
Methodology
We collected data from the CDC’s Behavioral Risk Factor Surveillance System (BRFSS). The BRFSS is the nation’s premier system of health-related telephone surveys that collect state data about U.S. residents regarding their health-related risk behaviors, chronic health conditions, and use of preventive services. We focused our research to only display data that concerned respondents who identified as Veterans.
Although the data we have compiled is from a government source, it does rely on self-report. Self-reported data can have many issues. These issues can include selective memory, telescoping, attribution, exaggeration, etc.
Fair Use Statement
If you or your readers are concerned about the Vet health crisis in America, we encourage you to share the results of our study on your site for any noncommercial use. Include a link back to this page so your readers can see our complete findings and our contributors earn credit for their work, too.